When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Pregnancy Sleep Positions
- Experts recommend sleeping on the left side during pregnancy to increase blood flow to the uterus and fetus.
- Sleeping on your back or stomach during pregnancy is only considered safe during the first trimester.
- Using pillows for support can make adjusting your sleep position during pregnancy easier and help you get better sleep.
Nighttime bathroom trips, nausea, heartburn, lower back pain, leg cramps: There are a number of things that complicate sleep during pregnancy. And as their bodies grow and change to accommodate the fetus, many pregnant people have trouble finding a comfortable sleep position. Unsurprisingly, these factors can make it difficult to obtain enough high-quality sleep.
Below, we examine the best pregnancy sleeping positions and discuss why experts recommend avoiding certain sleep positions during pregnancy. We also talk about how pregnant people can get comfortable so they can get the sleep they need.

Best Sleep Position During Pregnancy
Most experts agree that once the abdomen starts to expand, it’s best to sleep on the left side with knees bent (i.e., fetal position) . Not only is side sleeping more comfortable, it also helps improve blood flow for the pregnant person and the fetus . For added comfort and support, many pregnant people put a pillow between the knees or under the belly to relieve pressure on the lower back and hips.
Sleeping on the Left vs. Right Side
Both left- and right-side sleeping are generally considered safe during pregnancy, but the left side is often recommended as the better option.
Sleeping on the left side during pregnancy facilitates blood flow, ensuring that vital organs and the baby receive the nutrients and oxygen they need. This position also decreases the likelihood of swelling in the ankles and legs.
Right-side sleeping is still considered safe, especially if it’s more comfortable or if left-side sleeping isn’t sustainable throughout the night. Ultimately, whichever side helps you rest more soundly and wake up feeling better supported is a good choice.
Looking to improve your sleep? Try upgrading your mattress.
Back Sleeping During Pregnancy
During the first trimester, sleeping on your back is generally considered safe if that’s your usual position. However, as pregnancy progresses—particularly after 20 weeks—back sleeping can become problematic.
At this stage, the growing uterus can put pressure on the inferior vena cava, a major vein that carries blood back to the heart, which may reduce circulation to both the pregnant person and the fetus . This can lead to dizziness, shortness of breath, or lower blood pressure, so doctors typically recommend shifting to a side-sleeping position during the second and third trimesters.
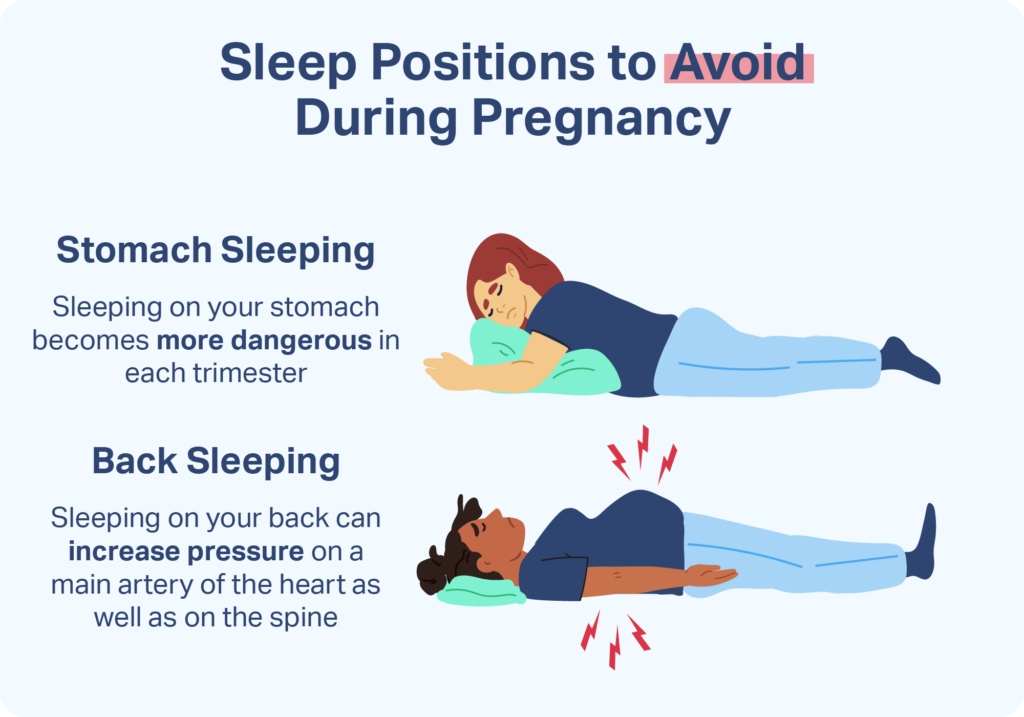
Sleep Positions to Avoid While Pregnant
Healthcare providers typically caution against stomach sleeping and back sleeping during the second and third trimesters of pregnancy.
As pregnancy progresses, back sleeping causes the weight of the uterus to place pressure on a main artery called the aorta and an important vein called the vena cava. This compression can make it harder for the heart to pump blood to the pregnant person and the fetus. Some pregnant people may experience discomfort and dizziness upon waking.
Moreover, back sleeping can put pressure on the spine. This position may lead to or exacerbate lower back pain, which affects a majority of pregnant people. Back sleeping is also associated with a higher chance of snoring , sleep apnea , or other breathing problems during sleep.
Though some experts say it’s best not to lie on the back from 20 weeks onward , a recent study found that back and right-side sleeping during the first 30 weeks of pregnancy probably did not raise the risk of stillbirth. Based on this research, some experts advise pregnant people to choose the sleep position that’s most comfortable for them during the first two trimesters of pregnancy.
How to Find a Comfortable Position
If you’re used to sleeping on your stomach or back, adjusting to side sleeping may be a challenge. Even if you normally sleep on your side, it can be difficult to find a comfortable sleeping position during pregnancy. However, there are some strategies that can help alleviate discomfort, increasing the likelihood of a good night’s sleep.
- Bend your knees: Healthcare providers recommend side sleeping with one or both knees bent, which can help support your back .
- Use pillows: To reduce discomfort and pain, you can put a pillow between your knees, against your lower back, or beneath your abdomen. You can also try a full-body pillow, many of which are designed specifically to support pregnant sleepers.
- Find a comfortable mattress or mattress topper: Materials that relieve pressure points, such as egg crate mattress toppers, may help relieve hip pain brought on by side sleeping.
- Elevate your upper body: If you have heartburn at night, try raising the head end of your mattress or bed. If you don’t have an adjustable bed, try a wedge pillow. Sleeping slightly upright may help relieve your symptoms.
- Sleep on the left side of the bed: You may be more likely to sleep on your left side if you move to the left side of the bed.
Sleep Better During Pregnancy
In addition to figuring out what position and configuration best support sleep during pregnancy, a number of other practices may help you sleep better.
Keep a Regular Sleep Schedule
Going to bed and waking up at the same time every day can help you take advantage of your natural sleep-wake cycle and fall asleep more easily. Additionally, enjoying a soothing beverage or a warm bath before bedtime can further reinforce sleep cues and signal to your body that it’s time to wind down. If you decide to take baths during pregnancy, be sure to ask your doctor about the appropriate temperature for your body and the fetus.
Make the Bedroom a Sanctuary
Reserving your bed for only sleep and sex helps limit unhelpful mental associations with work and other daytime activities. Removing bright lights, limiting noise, and keeping digital distractions out of the bedroom can also encourage sound sleep.
Nap as Needed
If you have trouble sleeping through the night, you can nap during the day to make up for lost rest. Ideally, naps should be taken earlier in the day to reduce negative impacts on nighttime sleep.
Help Your Baby Sleep Better With Pediatric Sleep Coaching

our partner at sleepdoctor.com
Learn More“Life-changing! My anxiety about my son’s sleeping habits were immediately reduced after talking to Sara. She went above and beyond to tailor a schedule to our goals, answer our questions, keep us on track, and check in to encourage us when we just thought we couldn’t do it anymore.”
Rachael B. – Verified Customer
Use Relaxation Exercises to Manage Stress
Stress prevents many pregnant people from sleeping soundly. Relaxation exercises may help calm your body in preparation for sleep. A health care provider can also provide resources to help navigate stress regarding pregnancy and upcoming life changes.
Minimize Food and Drinks in the Evening
While it’s important to stay hydrated throughout the day, drinking too many fluids or eating a big meal at night can make it harder to sleep. Small, plain snacks such as crackers might help ward off nausea during the night without exacerbating heartburn.
Limit Caffeine Intake
Caffeine interferes with sleep, so you may wish to reduce your consumption of coffee, tea, and caffeinated soft drinks. If you choose to drink caffeine during pregnancy, try limiting these drinks to the morning, when they are less likely to affect nighttime sleep.
Consider Prenatal Vitamins
Taking prenatal vitamins, such as iron and folic acid, not only helps the baby receive needed nutrients but may also alleviate the symptoms of restless legs syndrome, a sleep disorder that commonly affects pregnant people. Be sure to consult a health care provider before introducing any new supplements.
Exercise Regularly
Experts recommend that most pregnant people maintain a regular exercise routine throughout their pregnancy. Stretching and strengthening exercises, in particular, may help limit lower back pain and lower the chances of experiencing leg cramps. Targeting the trunk, abdominal, and back muscles may help your body better cope with the physical changes that take place during pregnancy.
When to Talk to Your Doctor
While it’s normal for sleep to become more difficult during pregnancy, persistent discomfort or trouble finding a safe, restful position may signal the need for medical guidance. You should reach out to your doctor if you’re frequently waking up on your back in the second or third trimester and feeling dizzy, short of breath, or nauseated.
It’s also important to talk to your doctor if you’re experiencing ongoing back or hip pain, swelling, poor sleep, or other symptoms of a sleep disorder, as some conditions have been linked to a higher risk of pregnancy complications.
Your provider can recommend strategies, positional adjustments, or supportive sleep products to help improve your rest and protect both your health and your baby’s development. They can also provide diagnosis and treatment for pregnancy-related sleep disorders like obstructive sleep apnea, heartburn, or restless legs syndrome.
Frequently Asked Questions
Can you sleep on your back while pregnant?
Sleeping on your back is generally considered safe during the first trimester. However, starting around 20 weeks, back sleeping may put pressure on major blood vessels, potentially reducing blood flow to you and your baby. Most experts recommend side sleeping in the second and third trimesters to avoid these risks.
Can you sleep on your stomach while pregnant?
Sleeping on your stomach is typically safe early in pregnancy, but it becomes uncomfortable and impractical as the belly grows. While there’s no harm in stomach sleeping during the first trimester, most people naturally shift to side sleeping as their body changes.
What’s the best sleeping position for hip pain while pregnant?
Sleeping on your side with a pillow between your knees can help reduce pressure on the hips and align the spine. A pregnancy pillow that supports the belly and back may also help relieve hip pain and improve sleep comfort.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
12 Sources
-
Cronin, R. S., Li, M., Thompson, J., Gordon, A., Raynes-Greenow, C. H., Heazell, A., Stacey, T., Culling, V. M., Bowring, V., Anderson, N. H., O’Brien, L. M., Mitchell, E. A., Askie, L. M., & McCowan, L. (2019). An individual participant data meta-analysis of maternal going-to-sleep position, interactions with fetal vulnerability, and the risk of late stillbirth. EClinicalMedicine, 10, 49–57.
https://pubmed.ncbi.nlm.nih.gov/31193832/ -
A.D.A.M. Medical Encyclopedia. (2020, June 2). Problems sleeping during pregnancy. MedlinePlus.
https://medlineplus.gov/ency/patientinstructions/000559.htm -
The Manual’s Editorial Staff. (2022, September). Overview of blood. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/quick-facts-blood-disorders/biology-of-blood/overview-of-blood -
Lockwood, C.J. & Magriples, U. (2022, October 13). Prenatal care: Patient education, health promotion, and safety of commonly used drugs. In V. Berghella (Ed.). UpToDate.
https://www.uptodate.com/contents/prenatal-care-patient-education-health-promotion-and-safety-of-commonly-used-drugs -
Anderson, N. H., Gordon, A., Li, M., Cronin, R. S., Thompson, J., Raynes-Greenow, C. H., Heazell, A., Stacey, T., Culling, V. M., Wilson, J., Askie, L. M., Mitchell, E. A., & McCowan, L. (2019). Association of supine going-to-sleep position in late pregnancy with reduced birth weight: A secondary analysis of an individual participant data meta-analysis. JAMA Network Open, 2(10), e1912614.
https://pubmed.ncbi.nlm.nih.gov/31577362/ -
Izci Balserak, B. (2019). Sleep-disordered breathing in pregnancy part 1. American Journal of Respiratory and Critical Care Medicine, 200(9), 18–19.
https://pubmed.ncbi.nlm.nih.gov/31674822/ -
Liu L, Su G, Wang S, Zhu B. The prevalence of obstructive sleep apnea and its association with pregnancy-related health outcomes: a systematic review and meta-analysis. Sleep Breath. 2019;23(2):399-412. doi:10.1007/s11325-018-1714-7
https://link.springer.com/article/10.1007/s11325-018-1714-7 -
Gersh, B. J. (2022, January 21). Maternal adaptations to pregnancy: Cardiovascular and hemodynamic changes. In C. J. Lockwood & B. J. Gersh (Eds.). UpToDate.
https://www.uptodate.com/contents/maternal-adaptations-to-pregnancy-cardiovascular-and-hemodynamic-changes -
Silver, R. M., Hunter, S., Reddy, U. M., Facco, F., Gibbins, K. J., Grobman, W. A., Mercer, B. M., Haas, D. M., Simhan, H. N., Parry, S., Wapner, R. J., Louis, J., Chung, J. M., Pien, G., Schubert, F. P., Saade, G. R., Zee, P., Redline, S., Parker, C. B., & Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (NuMoM2b) Study (2019). Prospective Evaluation of Maternal Sleep Position Through 30 Weeks of Gestation and Adverse Pregnancy Outcomes. Obstetrics and gynecology, 134(4), 667–676.
https://pubmed.ncbi.nlm.nih.gov/31503146/ -
The American College of Obstetricians and Gynecologists. (2021, December). Back pain during pregnancy.
https://www.acog.org/womens-health/faqs/back-pain-during-pregnancy -
Cronin, R. S., Chelimo, C., Mitchell, E. A., Okesene-Gafa, K., Thompson, J., Taylor, R. S., Hutchison, B. L., & McCowan, L. (2017). Survey of maternal sleep practices in late pregnancy in a multi-ethnic sample in South Auckland, New Zealand. BMC Pregnancy and Childbirth, 17(1), 190.
https://pubmed.ncbi.nlm.nih.gov/28623890/ -
Bermas, B. L. (2022, June 22). Maternal adaptations to pregnancy: Musculoskeletal changes and pain. In C. J. Lockwood (Ed.). UpToDate.
https://www.uptodate.com/contents/maternal-adaptations-to-pregnancy-musculoskeletal-changes-and-pain
















